Copyright 2025
Medical Security Card Company, LLC
All Rights Reserved
We take the privacy of your personal information seriously. By signing up I agree to WellRx's terms of use and privacy policy.
By Rosanna Sutherby, PharmD
July 29, 2020
American pharmacies have come a long way from the years of colonial apothecaries to the modern automated pharmacies of today. Evolution in pharmacist education and changes in the legislature has shifted the roles of pharmacists. Read on for a brief history of pharmacies in the United States.
In 1630, Governor John Winthrop, founder of Boston, hired British apothecary Robert Cooke to assist him in preparing remedies using herbs imported from England and other natural ingredients.
In 1729, the Irish immigrant Christopher Marshall opened one of the first apothecaries in colonial America. It was located in Philadelphia. For 96 years, the Marshall Apothecary served as a community pharmacy as well as a training ground for aspiring pharmacists. Marshall’s granddaughter, Elizabeth Marshall, took over the store in 1805 and became the second American female pharmacist. The first was Elizabeth Gooking Greenleaf, who bought and ran an apothecary in Boston in 1727.
In 1821, almost 100 years later, the first pharmacy school, Philadelphia College of Pharmacy, opened. Shortly after, in 1852, the first national pharmacy association, the American Pharmaceutical Association (APhA), was established.
Initially, the way into the profession of pharmacy was through apprenticeship. Someone interested in pharmacy would train under the tutelage of an established pharmacist. The opening of the first pharmacy school shifted education to formal institutions, and even these institutions underwent several changes over the years. Early colleges offered a Graduate in Pharmacy (Ph.G.) degree, which could be turned into a Pharmaceutical Chemist (Ph.C.) degree with an additional year of study.
By the 1940s, the Bachelor of Science in Pharmacy (B.S.Pharm.) was introduced, and in 1997, the Doctor of Pharmacy (Pharm.D.) six-year program became the only accredited pharmacy degree.
Early American pharmacies were referred to as apothecaries, and pharmacists were often called druggists or chemists. The role of the pharmacist then included preparing and dispensing remedies and counseling patients. By the 19th century, Edward Parrish of the APhA standardized the name “pharmacist” for all pharmaceutical practitioners. Until the 1950s, pharmacists prescribed, made, and dispensed medicines and provided patient counseling.
The passing of the 1951 Durham-Humphrey Amendment to the Federal Food, Drug, and Cosmetic Act of 1938 shifted the role of pharmacists. Until then, pharmacists were able to prescribe and dispense any medication except narcotics. The Durham-Humphrey Amendment restricted pharmacists to dispensing medications only with a physician’s prescription. Pharmacist recommendations were limited to over-the-counter (OTC) medications, and their role shifted to dispensing drugs and ensuring medication safety.
In the 1980s, a movement toward clinical pharmacy began to expand the role of pharmacists. By 2003, the Medicare Prescription Drug Improvement and Modernization gave pharmacists the ability to, once again, counsel patients on prescription drugs as well as OTC medications. The clinical pharmacy movement expanded the pharmacist’s role in the community pharmacy to include administering vaccines, counseling patients, and other patient care services. Pharmacists now can focus on disease and chronic condition management, medication management, health and wellness, and other services that help improve patients’ quality of life.
The role of modern-day community pharmacies differs from that of the apothecaries of colonial America. Pharmacists of colonial apothecaries prepared most of the remedies that they dispensed. By 1900, the industrial revolution introduced new forms of medications, such as tablets, gelatin capsules, and enteric-coated pills. These medication forms were mass-produced and lined the shelves of pharmacies of the 1900s. However, compounded medicines, including liquids, creams, ointments, lotions, eye drops, and eardrops, were still common. Today’s pharmacies are largely automated, with robots that count and bottle commonly used medicines, and compounding has become less common.
Record-keeping in the pharmacy has also seen significant advances. Pharmacists have moved from handwriting all prescriptions to using systems in which prescriptions are transferred electronically directly from the prescriber’s office to the patient’s community pharmacy.
To keep track of patient records, pharmacists handwrote all the patients’ prescriptions on index cards that used carbon to transfer the information to receipts. Today’s pharmacies keep electronic patient records.
As the roles of community pharmacists have evolved over time, so have those of pharmacy technicians. The support staff of precomputer pharmacies consisted mainly of cashiers. The introduction of computers in the pharmacy shifted the pharmacy support role from cashier to pharmacy technician. Technicians now are responsible for more than ringing up sales at the register. They can input prescriptions in the computer, answer telephone calls, and assist the pharmacist in preparing medications and setting up immunizations.
Pharmacies today can include patient care areas where pharmacists can provide various clinical patient care services. Clinics with prescribing practitioners inside the stores are becoming more prevalent. The role of pharmacists in community pharmacies has come full circle from colonial times, but today’s highly automated and computerized pharmacies are quite different from yesteryear’s nostalgic apothecaries.
Rosanna Sutherby is a freelance medical writer who has been a practicing pharmacist in her community for close to 20 years. She obtained her Doctor of Pharmacy from Nova Southeastern University in Ft. Lauderdale, FL. She utilizes her clinical training in the pharmacy, where she helps patients manage disease states such as asthma, diabetes, heart disease, hypertension, and many others. Dr. Sutherby reviews and recommends drug regimens based on patients’ concurrent conditions and potential drug interactions.
References:
https://aihp.org/wp-content/uploads/2018/08/1-Early-Pharmacy-in-America.pdf
http://www.pharmacy.auburn.edu/about/pdf/history-pictures.pdf
https://www.aphafoundation.org/sites/default/files/ckeditor/files/WIP%20mural%20descriptions.pdf
https://brewminate.com/a-brief-history-of-the-pharmacy-in-the-united-states/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4821736/
https://www.stlcop.edu/practice/about.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6789634
https://www.pharmacytoday.org/article/S1042-0991(16)30677-6/fulltext

For your convenience, use the ScriptSave® WellRx mobile app. Now savings are well in hand, right at the pharmacy counter. Save on your family's prescription medicines.
Learn More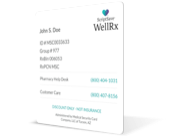
Your choice. Get a ScriptSave WellRx Savings Card. Or Download the free mobile app from the App Store or Google Play Store
Get A Card
ScriptSave WellRx Grocery Guidance leverages leading-edge nutritional data science to help you know which food products on your grocery store shelf are truly good for YOU.
Healthy Foods For YouTags:

August 03, 2020

July 28, 2020

July 27, 2020
You need to log into the site to use this feature
This feature requires registration. Sign up or log in to your free WellRx account to gain access to this and other tools to help make managing your medications and wellness easier.
Benefits Include:
 Store & manage your medication list
Store & manage your medication list
 Medication pricing updates
Medication pricing updates
 Medication information
Medication information
 Pill & refill reminders
Pill & refill reminders
 Medication journal & mood log
Medication journal & mood log
This feature requires registration. Sign up or log in to your free WellRx account to gain access to this and other tools to help make managing your medications and wellness easier.
Benefits Include:
 Store & manage your medication list
Store & manage your medication list
 Medication pricing updates
Medication pricing updates
 Medication information
Medication information
 Pill & refill reminders
Pill & refill reminders
 Medication journal & mood log
Medication journal & mood log
You will be redirected to your program in 5 seconds.
Our Terms and Conditions and Privacy Policy have recently been updated.
By declining you will be logged out of your account